In the hunt for improved antibiotics, it is important to realize that natural products have been, without question, the most prolific source of all medicines. With the advent of massively parallel DNA sequencing, it has become apparent that our knowledge of natural product structure and function is astonishingly incomplete. Exploration of uncharted natural product chemical space will undoubtedly lead to improved, and entirely new, medicines. Thus, our group focuses on elucidating the biosynthesis, structure, and function of natural products. Our primary focus has been on thiazole/oxazole-containing peptides. Characterized examples have activities ranging from antibacterials to virulence-promoting toxins. Therefore, the study of these peptidic natural products allows us to not only better understand bacterial virulence (where pharmacological intervention would constitute a pathogen-specific approach to bacterial infection) but also explore unique chemical architectures, ideally positioning us to introduce new structural classes of antibiotics. Our recent successes and focal areas are highlighted below by research project.
anti-virulence
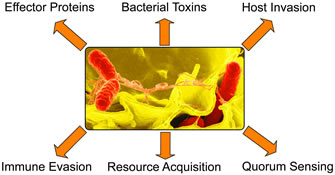
Bacterial pathogens wield an arsenal of virulence factors that permit the establishment and persistence of disease. Taking the logic of the “ultra-narrow” scenario one step further, another strategy for suppressing the rise of antibiotic resistance would be to have a drug that does not kill (nor suppress the growth of) bacteria. Instead, the drug would function via targeting a lynchpin virulence factor, rendering the pathogen incapable of causing disease. Relative to conventional antibiotics, an anti-virulence strategy will delay the development of antibiotic resistance by at least two routes: (i) Because disease-causing bacteria employ disparate pathogenic mechanisms, anti-virulence agents will be inherently ultra-narrow spectrum, negating the evolutionary advantage of laterally transferring resistance cassettes; (ii) Instead of forcing the pathogen to “mutate or die”, it is rendered non-pathogenic and should be cleared from the host like any other bacterium. This reduces the selection of random mutations that diminish drug efficacy.
As attractive as this strategy may seem, it is not without risk or opposition. Critics suggest that it could be dangerous to leave bacteria alive inside the patient. This certainly could be the case with systemic infections, but in general, bacteria, even disease-causing species, are constantly colonizing most parts of the body with no ill effects (only under rare occurrences is a pathogenic attack initiated). Until virulence-targeting drugs are fully evaluated through clinical trials, the utility of such drugs will remain theoretical.
We are working on developing and characterizing antivirulents as a new class of anti-infectives.
recent publications
- Maxson, T., et al., "Targeted treatment for bacterial infections: Prospects for pathogen-specific antibiotics coupled with rapid diagnostics." Tetrahedron (2015). doi:10.1016/j.tet.2015.09.069
- Molloy, E.M., et al., "Identification of the minimal cytolytic unit for streptolysin S and an expansion of the toxin family." BMC Microbiol. (2015). doi:10.1186/s12866-015-0464-y
- Maxson, T., et al., "HIV protease inhibitors block streptolysin S production" ACS Chem. Biol. (2015). doi:10.1021/cb500843r